Terminology Won't Save Us
Rethinking the trans competence training.
As a trans person, I’ve seen many iterations of language over the years. Each one seemed to be the answer; each one caused another problem.
At various Trans 101 sessions, we used to hand out glossaries that were pages long. We thought that if people knew the right words, the right terminology, this would result in greater equity.
I now see this as a dangerously unproven hypothesis.
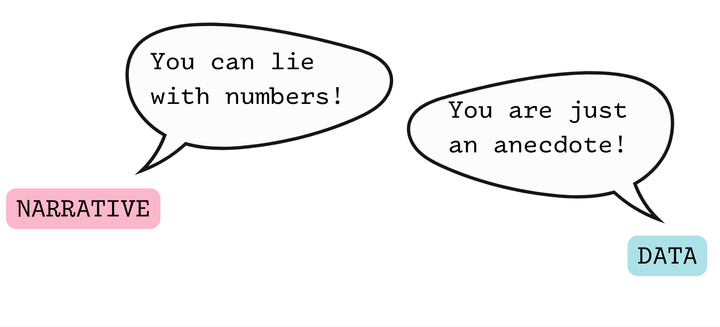
It’s not entirely clear that teaching terminology does anything for equity or patient experience at all.
I’ve never seen any data on it. I’ve seen some data to show staff-reported outcomes in terms of knowledge or preparedness to treat trans patients, but this isn’t the same thing at all. If your trans patients aren’t having a good experience, it doesn’t matter how much training you did or how much your staff supposedly learned.
As a trans person, I can tell you that I have received compassionate and understanding care from healthcare workers who had not received any particular training about trans issues. These healthcare workers understood that I was a human in need of help, that I was a trans man, and that they were in a position to help me.
I’ve shared elsewhere about the medical billers who stepped up and helped me resolve a disturbing series of gender-related insurance denials during my first pregnancy. I’m not sure how much terminology they knew. But I don’t think it was knowledge of terminology that led them to be patient and reassuring toward me and to refile my paperwork and fight with my insurer for as long as it took.
I think that required compassion, professional competence, and determination. When do we teach these in our competence trainings?
On the other side, I have received patronizing, awkward, and uncomfortable care from those who have received extensive trans competence trainings. I have been asked my pronoun what felt like every five minutes, despite it being in the chart, with staff huffily saying, “Well, I just didn’t want to assume!” I have had call center employees at my insurance plan patronizingly and incorrectly explain to me the difference between sex and gender. I have had providers so afraid of making a mistake related to my gender identity that their hands were literally shaking.
Surely this isn’t the desired outcome of these trainings?!
And if we’re missing the mark so badly, surely it’s time to think of another approach. Perhaps one that empowers providers and staff as communicators, critical thinkers, and advocates, providing the trans-specific knowledge they need within this broader context of problem-solving and advocacy.
But I have another concern about these terminology-based trainings.
Extensive data shows us that people subconsciously make associations and think in metaphors. So then, what are the implications of suggesting that trans people’s lives and needs are so complex that a glossary or detailed understanding of terminology is essential in understanding them?
Might this emphasis on terminology have the effect of reducing compassion toward trans people, or encouraging an overfocus on scripted behaviors rather than attending to the patient in front of you?
And then there’s the question of why we’ve gravitated toward terminology.
I recently attended a conference on LGBTQ+ health that was primarily for healthcare workers and medical trainees. Despite the fact that this conference was specifically geared toward those with a strong professional interest in LGBTQ+ health, many presentations included several slides about “terminology,” such as the difference between sex, sexual orientation, and gender identity, and about basic approaches to cultural competence, such as “not making assumptions.”
“Just to review these, in case anyone isn’t aware,” said one presenter, before launching into basic definitions around sexual orientation and gender identity.
I wondered: At the American Statistical Association meeting, do they routinely include a basic slide or two about probability theory, “in case anyone isn’t aware”?
(My friend, a prominent biostatistician, assured me that they do not.)
What, then, is wrong with our field, that we continue to review these basics, even in spaces primarily geared toward experts?
Whose interests does this serve?
Not mine, I can assure you. Not mine as a professional, and not mine as a trans patient.
This emphasis on terminology both lowers the bar on what true competence and compassionate care means, and discourages critical thought about the genuine needs of the trans community and how one might creatively solve them.
We need to start with compassion and advocacy. The necessary words will follow.